This is What Sickle Cell Disease Looks Like: The Research Perspective
Eric Low, a thought leader in rare disease research, speaks on the need for better collaboration across health stakeholders to improve SCD outcomes.
Having friends or family who suffer from an invisible condition like Sickle Cell Disease can make it real for many.
For Eric Low, this is particularly true. One of his close friends, a brilliant mind in SCD innovation, lost his life after having a severe vaso-occlusive crisis. He was never able to see others in the SCD community benefit from his pioneering research. Another patient and friend of Eric’s is working to accelerate research in SCD. Their motivations are aligned, as well as the questions they pose to peers in the SCD research community. Recently, Eric was asked:
“What do you think the journey to a cure looks like?’. For me, I can see why this is a really important question which warrants a well thought-through response.”
“Is there someone developing a silver bullet for SCD? I’m not sure. However, there are a number of great companies on this journey from gene-editing technology to novel new treatment options for patients.”
In his tenure leading rare disease research organisations like Myeloma UK, Eric has had much time to reflect on why we haven’t yet found a cure. Eric believes that it is too simple to say that the complexity of Sickle Cell Disease has hindered us in finding a cure for SCD. It is, in fact, the lack of collaboration and pace that has prevented us from doing so.
Care for SCD patients require care that is both integrated and personalised to prevent disease progression and deterioration. Due its lack, alongside absent collaboration and pace, we are starting to see increasing admission rates of patients with higher disease complexity.
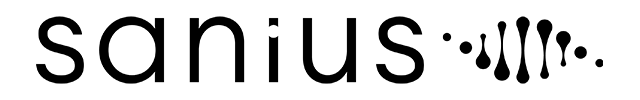
Data taken from the largest 10 treatment centres show that although diagnosis depth has generally decreased, more and more patients are presenting with highly complex conditions. Patients and clinicians report an increased number of co-morbidities since 2018, suggesting that current pathways are not meeting their care needs. Eric adds that this is representative of the fact that we are yet to provide effective enough treatment for patients; especially given the varying complexity of each person’s condition:
“My view is that while there probably have been a number of significant advances and improvements, things are still pretty much the same. For SCD patients, they still face the same hurdles, challenges and trip hazards that they have always had. They will see themselves facing these challenges again and again unless we do something to move SCD care forward.”
“However”, Eric adds, “it is 2022. We still haven’t achieved the things we set out as far back as 2008, and we need to question why.”
Like many in the SCD community, Eric is frustrated that it has taken over 20 years for us to see any momentum in SCD; let alone a substantive cure. As it stands, improved care strategies and emphasis on blood donations are no longer enough to stem staggering rates of SCD health inequalities and rising number of diagnoses.
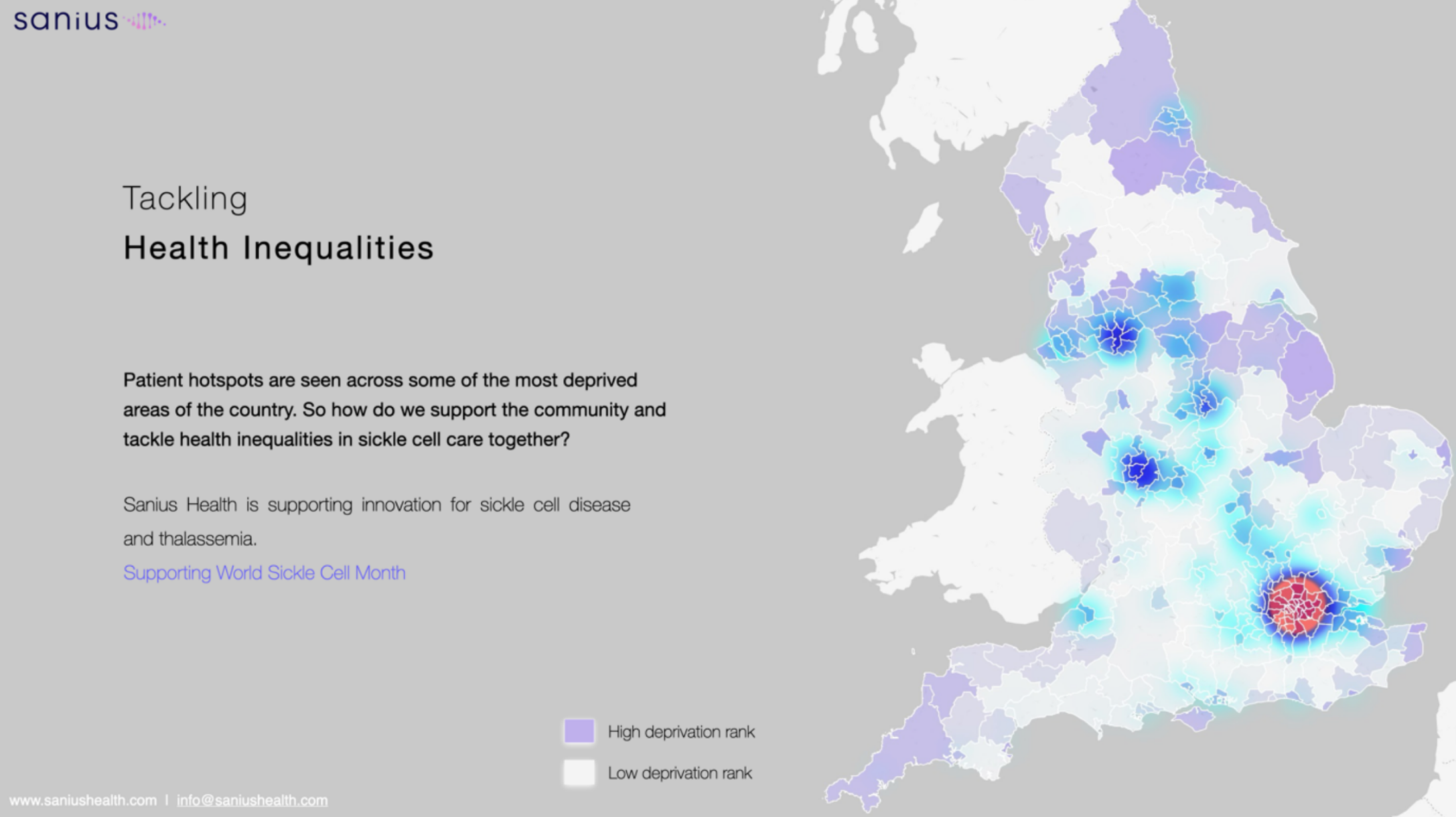
In the UK alone, there are roughly 15,000 patients with SCD. Many of these patients are located in some of the most deprived areas of the country and present with higher disease complexity. For them, outcomes are dangerously low and life threatening. Given current health inequalities and outcomes, Eric believes that the only way forward for patients is to receive a cure:
“Although they may provide some relief to patients, the treatments we have today aren’t transformational. They will help with pain; they will help with the quality of life. They might even prevent the onset of vaso-occlusive crises.”
“But they’re not silver bullets and certainly not a permanent cure by any stretch of the imagination.”
Eric is cognizant that ‘in reality, very few things are curable’, and despite the concerted efforts to progress SCD treatments, we are still in unchartered territory in finding a substantive cure. This is due to a lack of alignment regarding resources, intelligence and efforts that genuinely focus on developing a viable cure for SCD. Current approaches, which Eric likens to “throwing spaghetti against a wall and hoping it sticks”, are no longer enough for patients.
“If we’re really serious about making substantive improvements in SCD outcomes, whether that is through living well with a disease or finding a cure, we need a universally agreed blueprint or approach. I think we must combine a critical mass of resource and intelligence approaches to find common ground – not just within SCD, but also within different therapeutic areas.”
He stresses that the “blueprint towards a cure” will take every single stakeholder coming together to tackle SCD, from those representing: the medical community, patient communities, research organisations and governing bodies. As he states, making a real impact for SCD patients will take moving mountains to get the right people in the room
“Cures for conditions like SCD do not magic out of thin air. You’ve got to write a blueprint, and you need to get the right people with the right expertise in the same room so that the right incentives for bettering SCD care are applied across the health system”
“So I think we need to convene a panel of experts who represent various disciplines, from across the bench to bedside care. Whoever they are, our panel of experts must be able to look deeply into SCD’s most pressing problem statement: the fact that we need a cure. To get there, where do we start, and what steps do we take?”
Eric states that the only way the research community can navigate itself out of this stalemate is by working together and considering what patient data tells us. He urges experts to work together in examining the lived experiences of patients in order to define the criteria it will take to develop a cure. These include, and are not limited to applying intelligence, patient-reported-outcomes data and expert methodology for developing research pathways:
“Finding a cure, or even improving SCD patient outcomes, is not just about science. It’s about investment. It’s about consortia. It’s about alignment. It’s about getting the information and incentives in the right places, and involving all stakeholders in research design and every step of the pathway.”
“By answering these questions’, Eric adds, we can begin to test our thinking around treatments, cures and mechanisms; or at least pathways that aren’t going to fall over in later research phases”
Regarding moving the needle on SCD treatments, promoting interconnectivity between stakeholders is close to Eric’s heart. He has seen first-hand the repercussions of misaligned research and investment efforts in SCD and other rare diseases. The result of absent interconnectivity, as Eric has witnessed, can result in the loss of innovation opportunities; or, worse even, the loss of lives:
“The road to an SCD cure, unless you’ve started on that road already, is 10, 20, 30 years away, will only appear if something serendipitous happens from left field.”
“If we do not focus our efforts, it will not be us who feels it: it will be our friends with SCD, the patients we treat and those who will come after them, who will pay the price. It is our duty to ensure that future generations will benefit from the innovation and research available to us – so that more lives can be saved”
To raise awareness of SCD, we are working with research leaders like Eric Low and other members of the SCD community to make improved SCD care a reality.
Learn more about raising awareness around Sickle Cell Disease by accessing Sanius Health’s campaign site: https://whatscdlookslike.com/